Four years ago, a SHP professor received a federal grant to work with the U.S. Department of Veterans Affairs (VA) to create a database of evidence linking toxic exposure from burn pits to diseases such as cancer and respiratory illnesses.
That work, led by Scott Parrott, director of SHP’s Methodology and Statistics Support Team, helped push forward the 2022 PACT Act—a landmark law that significantly expanded health benefits for veterans exposed to airborne toxins during their service.
Named for a decorated combat veteran who died from a rare lung disease after deployment in Iraq, the PACT Act marked a turning point for veterans suffering from conditions linked to toxic exposure.
Before the law, veterans had to prove their illness was directly caused by service in the Southwest Asia Theater of Operations—a difficult, often impossible task.
“We didn’t rewrite the law,” Parrott said. “But we were honored to contribute to an important change that now allows veterans to be presumed eligible for benefits if they develop certain respiratory illnesses after serving in high-risk areas.”
His VA grant was renewed this year and expanded. His team is now examining the relationship between toxic exposures and other conditions affecting Gulf War veterans, including interstitial lung disease, obstructive sleep apnea, and autoimmune disorders.
The effort began in 2021, when Parrott was asked by the VA to synthesize the scientific evidence linking military service to constrictive bronchiolitis, a rare but serious lung disease. Using a novel methodological approach, they challenged the framework previously used by the National Academies of Sciences, which had failed to establish a clear connection between exposure to burn pits and illness.
Their revised synthesis, submitted to the secretary of Veterans Affairs, was later presented to Congress—and helped influence change. In December 2024, the VA updated its clinical directives in accordance with the PACT Act, expanding health care for veterans who developed service-related health issues while deployed in the Persian Gulf region.
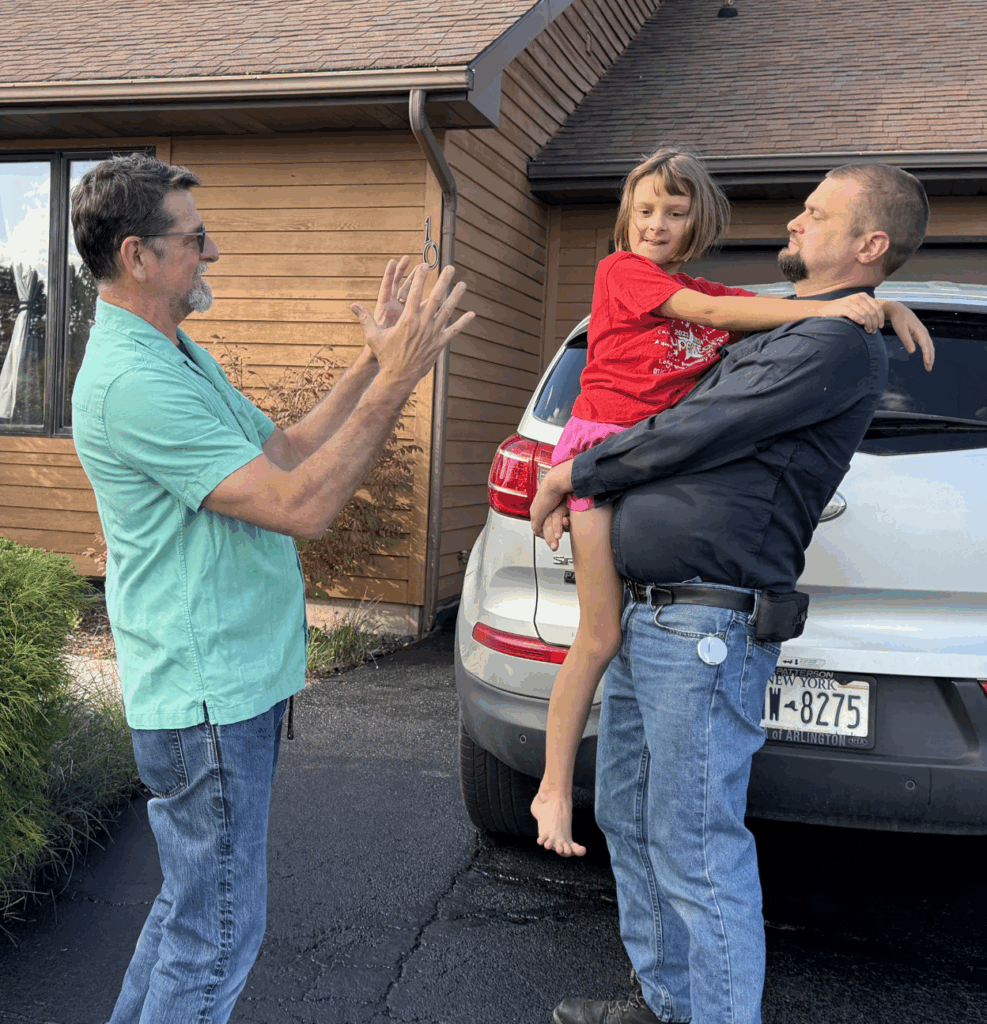
For Parrott, the work is deeply personal. His son-in-law, a veteran of multiple tours in Iraq and Afghanistan and later a military contractor in Kuwait, now suffers from chronic respiratory disorders and cardio-pulmonary problems. He was one of the thousands of veterans participating in the VA’s lung injury studies.
“When he came back from Kuwait, he had frequent infections, but never complained,” Parrott said. “Then one day I watched him struggle to carry boxes up the stairs, stopping to catch his breath, and it all clicked. He’s only in his mid-30s and can’t swim or hike or play on the trampoline with his daughter like he used to. It’s heartbreaking.”
Parrott’s work has also helped train the next generation of researchers. His project included 30 federal interns and eight from the Rutgers School of Pharmacy. Two of those interns have since joined the VA research staff.
His team is continuing to build systems that make it easier to keep scientific findings up to date, so new evidence can quickly reach researchers, policymakers, and military families. With the new funding, they’ve also been asked to expand the use of artificial intelligence to speed up and improve how they pull and combine military health data. This will help make the process faster and more accurate.
“This is really cutting-edge,” Parrott said. “And as an Army dad, it’s something I think is critically important.”