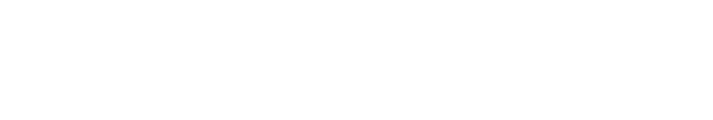
Welcome to Rutgers School of Health Professions
The nation’s largest, most comprehensive health professions school.
35+
health professions degrees and certificates
#7
Physician Assistant Studies ranked among Top 10
58%
of students are under-represented minorities
17%
of students
are fully online learners
Become the Next Generation of Health Professionals
From nutrition, lab sciences, and health informatics, to physical, occupational, and speech therapies; as well as psychiatric rehabilitation; our hands-on training and superior clinical experiences will prepare you to deliver exceptional patient-focused care.
NEWS
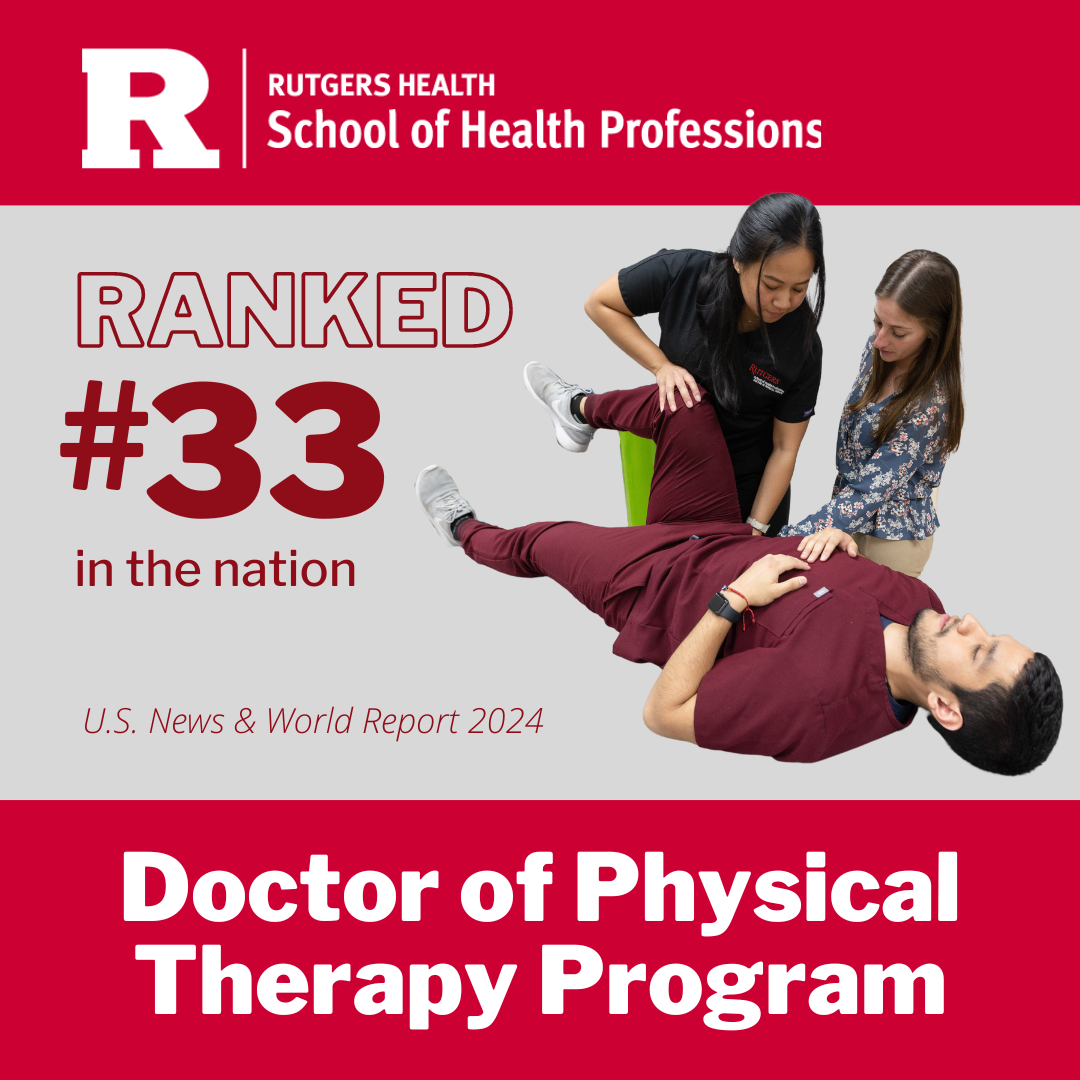
SHP’s Doctor of Physical Therapy Program Ranks #33 in the Nation
#1 in New Jersey and #2 in Tri-State Area
 […]
[…]
Eye2Eye Peer Support Offers Vital Connection for the Visually Impaired
 Tracey Simon, a peer support specialist, understands the devastating toll of vision loss. When she lost her […]
Tracey Simon, a peer support specialist, understands the devastating toll of vision loss. When she lost her […]
Investigating Running Injuries
 High school cross-country runners from across New Jersey are helping SHP researchers learn whether certain factors are predictors of running injuries.
High school cross-country runners from across New Jersey are helping SHP researchers learn whether certain factors are predictors of running injuries.
Allison Brown, assistant professor in physical therapy and principal investigator, is working on the study with collaborators Andrew Lynch, […]
EVENTS
Rutgers School of Health Professions Research Tower
Learn More ›
Busch Campus in Piscataway and College Avenue and Cook/Douglass Campuses in New Brunswick
Learn More ›